PNB : Peripheral Nerve Block
Ultrasound has been the primary tool in Peripheral Nerve block (PNB). The utility of ultrasound to facilitate a range regional anesthesia techniques including brachial plexus and femoral blocks .
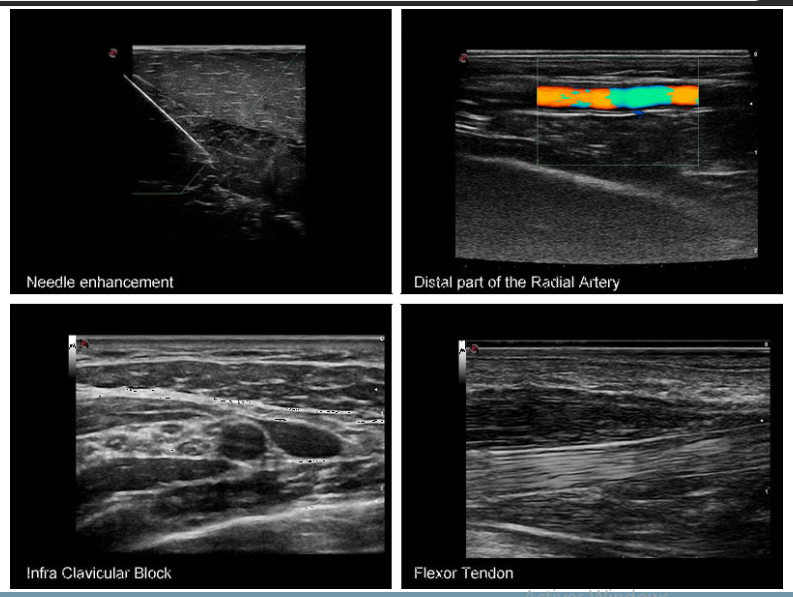
A wireless portable ultrasound probe with a built in needle guide offers more control for anesthesiologist while performing PNB.
A mini linear with high frequency transducer allows visualization of the anatomy of the region of interest.
This allows more informed guidance for the needle pathway to the target while avoiding structures that might be damaged by the needle.
The wireless ultrasounds also allow visualization of the needle tip as it is passed through the tissues, confirming alignment with the intended path, again reducing the likelihood of inadvertent needle trauma to unintended structures.
Moreover, for PNB the portable ultrasound scanner real-time ultrasound imaging permits continual visualization of local anesthetic solution delivery to ensure proper distribution, with the potential for adjustment of the needle tip position as necessary to optimize local anesthetic distribution.
Ultrasound-guided PNB may be broken down into two fundamental aspects: imaging structures in the plane of section, including the target nerve, and guiding the needle. Nerve imaging may be performed in either short-axis (probe face perpendicular to axis of nerve) or long-axis (probe face parallel to axis of nerve) position
As anatomic recognition remains essential to placing blocks with real time visual guidance. To optimize the ultrasound image, the mnemonic PART (pressure, alignment, rotation, tilting) is recommended. Pressure is necessary to minimize the distance to the target and compress underlying subcutaneous adipose tissues.
Alignment refers to placing the transducer in a position over the extremity (or trunk) at which the underlying nerve is expected to be in the field of view. Rotation allows fine-tuning of the view of the target structure. Tilting helps to bring the face of the probe into a perpendicular arrangement with the underlying target to maximize the number of returning echoes and thus provide the best image.
Reference: Introduction to Ultrasound-Guided Regional Anesthesia.
[launchpad_feedback]
Disclaimer: Although the information we provide is used by different doctors and medical staff to perform their procedures and clinical applications, the information contained in this article is for consideration only. SIFSOF is not responsible neither for the misuse of the device nor for the wrong or random generalizability of the device in all clinical applications or procedures mentioned in our articles. Users must have the proper training and skills to perform the procedure with each ultrasound scanner device.
The products mentioned in this article are only for sale to medical staff (doctors, nurses, certified practitioners, etc.) or to private users assisted by or under the supervision of a medical professional.


